TORONTO — Hospitals in smaller and rural Ontario communities have been recruiting, training, and poring over schedules in the hopes of avoiding another summer wave of temporaryER closures – though the problem never really went away.
Staffing shortages led hospitals to close their emergency departments for hours or even days at a time during the summer of 2022.
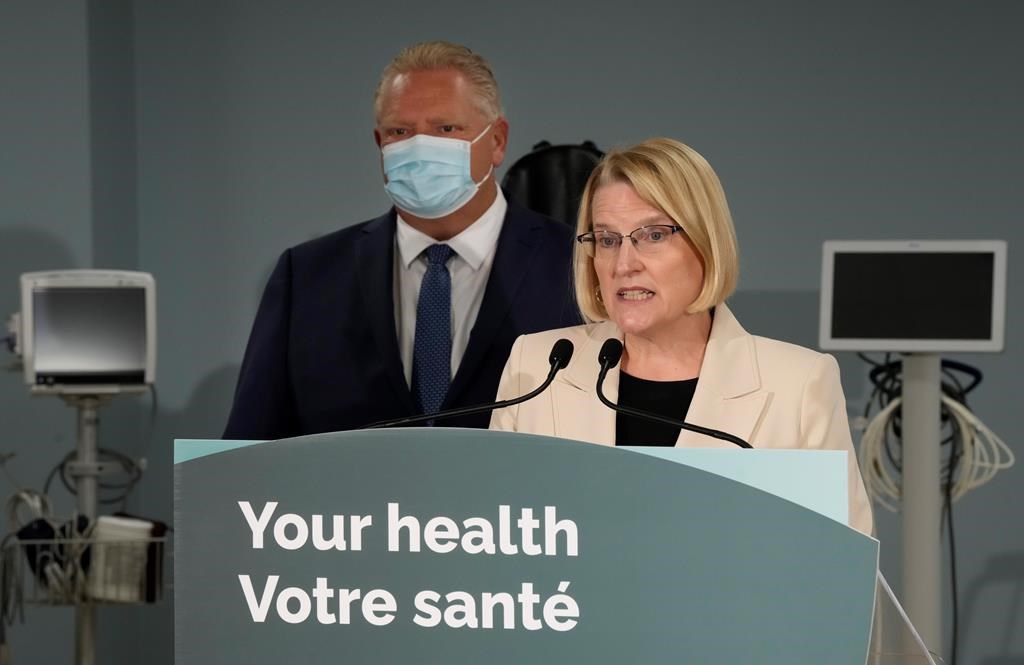
Health Minister Sylvia Jones noted at the time that similar staffing challenges and closures were seen across the country, and that there was a high rate of health-care workers taking well-deserved vacation time.
But the closures did not stop at the end of the summer vacation period. South Bruce Grey Health Centre had overnight ER closures at all of its four sites through the fall, and had to fully close its Chesley ER for two months. The hospital has noted a shortage of nurses there since before the pandemic and the site still only operates Monday to Friday, during the day.
Other temporary closures were reported in the province during the winter, and now, just as the summer season is due to arrive, there have been more than half a dozen closures in recent days – including for 48 hours recently in Thessalon, a town in northern Ontario.
“I would be surprised if it’s the only one (this summer) and I’m not happy about having to say that,” said North Shore Health Network president and CEO Tim Vine.
The network has hospitals in Thessalon, Blind River and Richards Landing, Ont.
“It’s obviously something that we agonize about and we do everything we possibly can to avoid, but I don’t see any other way through the summer without having some closures, and they will almost certainly not be limited to Thessalon,” he said.
Thessalon has been without a primary care physician for about two years, contributing to higher ER volumes. It has been relying on doctors from other communities to serve the hospital on a temporary basis, but those can be hard to attract, Vine said.
In Minden, Ont., the hospital has decided to permanently close the local ER as of June 1, due to staff shortages. It saw no closures last summer, but Carolyn Plummer, president and CEO of Haliburton Highlands Health Services, said there were many close calls that would have led to short-notice temporary closures of either the Minden or Haliburton ERs – or both.
“While there were shortages prior to the COVID-19 pandemic, they were significantly exacerbated by the pandemic, which did require HHHS to turn to nursing agencies to fill scheduling gaps,” Plummer wrote in a statement.
“It is worse than last year. With no end in sight to these sorts of staffing shortages, HHHS had to make the difficult decision to consolidate emergency services at one location, in order to ensure it could maintain delivery of emergency services for all of Haliburton County.”
Like Haliburton Highlands and many other hospitals across the province, the Perth and Smiths Falls District Hospital has had to rely on nursing agencies to bolster staffing levels. That has left the eastern Ontario hospital with a stable staffing situation, but at a net cost of $2.8 million just last year, said president and CEO Michael Cohen.
“It is very expensive, but it’s also the price that we’re paying to keep services open,” he said.
Anthony Dale, president and CEO of the Ontario Hospital Association, said agency nurses have historically represented about one per cent of nursing hours in Ontario hospitals and more recently it has become about two per cent, but spending on them has risen by much more.
“The rates that some of the agencies are charging have ballooned completely,” he said. “They’re absolutely taking advantage of the situation and they’re taking advantage of the pandemic and the very demanding and punishing conditions that all health-care workers face.”
Dale said he is hopeful Ontario will see more emergency department stability this summer, as a lot of new programs and investments have started just in the last year.
But the situation in rural health care has been a long time coming, with successive governments failing to establish a coherent policy approach, he said.
“We’re rushing to make up for lost time and the government has implemented a wide range of well-designed and very constructive programs to recruit and retain, to incent health-care workers – and especially nurses – to consider practising in rural and remote communities,” Dale said.
“It’s just some of the underlying pressures are so significant that it’s proving to still be an ongoing challenge.”
A spokesperson for the health minister highlighted a number of programs and changes aimed at bolstering staffing, including covering the cost of nursing school tuition in exchange for working in the region individuals study in, automatically letting health-care workers from other provinces practise in Ontario and removing regulatory barriers for internationally educated nurses.
The Huron Perth Healthcare Alliance and its four hospital sites in southwestern Ontario have been making use of many of those programs, including one that gives new nursing graduates $25,000 if they work in an underserved area for two years. As well, they have been training staff outside the emergency department to be able to work there, and have introduced clinical coaches to support new graduates.
“We’re really trying to make our environment as conducive as possible to recruiting people and retaining them when they’re here,” said president and CEO Andrew Williams.
“In small hospitals, you’re one sick call away from potentially having to close and we faced that a number of times,” he said in a May 12 interview.
Four days later the hospital network’s emergency department in Seaforth had to close overnight, then again one week later, and again two days after that, and its St. Marys Memorial Hospital ER had to close overnight this past weekend.
This report by The Canadian Press was first published May 29, 2023.