TORONTO — Introducing a mask mandate when respiratory viruses surged in the fall may not have eased the crush on pediatric hospitals, a Public Health Ontario science brief obtained by The Canadian Press concludes.
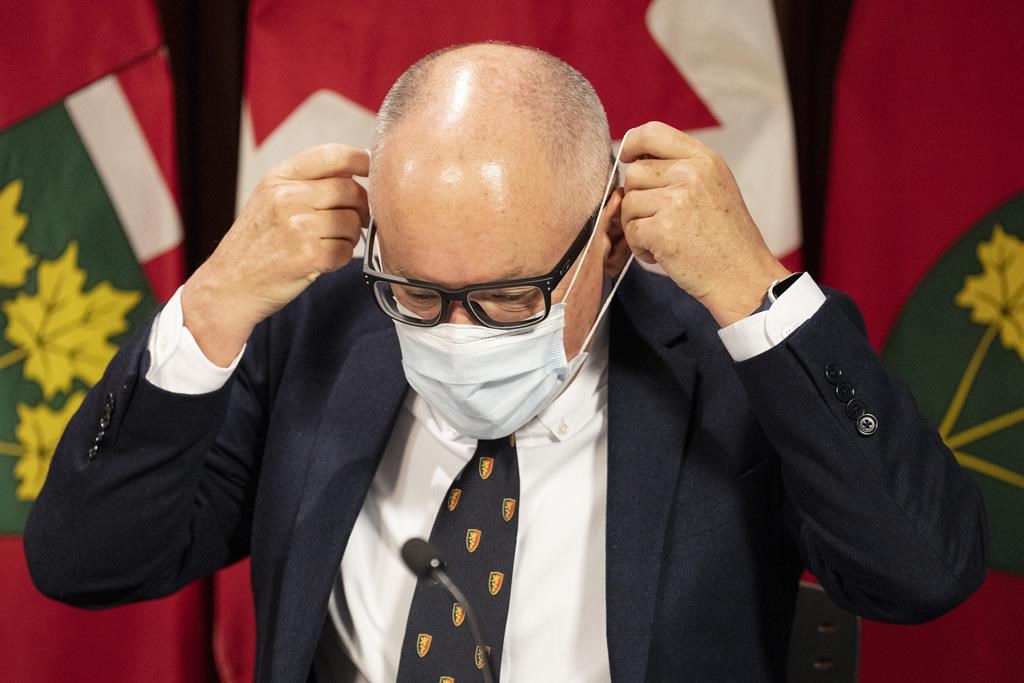
The brief – which was not proactively made public, unlike the reports done by the now-defunct science table predecessor – provides a glimpse of the evidence on which Chief Medical Officer of Health Dr. Kieran Moore made his decision to go no further than a “strong” recommendation on masking in mid-November.
The effects of masking on the transmission of COVID-19 are strong, the brief from late November notes. Mandates may not have produced more of a benefit than recommendations, its research suggests.
But with influenza and respiratory syncytial virus, or RSV, circulating at the time as well as COVID-19, the benefits of mask mandates became less clear for the group of experts.
“Current evidence suggests that adherence to masking, in addition to other layered measures such as self-screening, staying home when ill, and vaccination, are likely to prevent transmission of influenza, RSV and COVID-19 in children and youth, especially in indoor community settings where transmission is high,” the PHO document concludes.
“Given the number of respiratory viruses currently in circulation, there is less certainty about the potential magnitude of the effect on transmission.
“It is also uncertain whether potential decreases in transmission are sufficient to reduce pediatric emergency department visits, hospitalization, and ICU admission to preserve capacity within the health-care system.”
That brief settled the debate for the province’s top doctor.
“The body of evidence for strictly implementing a mask mandate wasn’t there,” Dr. Moore told The Canadian Press in a recent interview.
“In no jurisdiction has there been a mandatory masking recommendation, nor has our expert panel recommended that to us.”
Moore said he does not see a mask mandate now or in the future.
In mid-November, Moore wasn’t so sure.
Respiratory viruses led to a massive surge in young patients who needed hospitalization. Intensive care units and emergency departments at the major children’s hospitals across the province saw historic volumes from October to December.
The surge forced children’s hospitals in Toronto, Ottawa, Hamilton and London, Ont., to cancel surgeries in order to free up staff and beds to deal with the problem.
On Nov. 14, Moore held a news conference where he “strongly” recommended the public wear masks in indoor settings to protect children from circulating respiratory viruses. He said he was discussing and reviewing the possibility of mandating masks in schools again.
That same day, Moore’s office requested help from Public Health Ontario.
“The Office of the Chief Medical Officer of Health requested a summary of evidence on the effectiveness of mask-wearing, particularly among children and youth, in the context of circulating influenza, RSV and COVID-19,” the brief said.
“Information about public acceptability of mask mandates was also requested.”
Ten days later, Public Health Ontario responded with a 14-page brief.
There was little evidence in scientific literature on the sole effects of masking on the transmission of influenza and RSV, it notes.
“We were unable to identify data on the effectiveness of community-level masking in preventing transmission of influenza or RSV,” the document says.
“However, widespread mask use in general or targeted populations may be expected to reduce the rate of transmission of viral respiratory pathogens in the community.”
The effects of masking on the transmission of SARS-CoV-2 – the virus that causes COVID-19 – is much stronger, the document notes, including evidence by the province’s now-defunct science table.
“It reported that mask mandates were associated with a lower incidence of SARS-CoV-2 infection compared to schools without mask mandates,” the document says.
The brief references a Public Health Ontario synthesis of research in March 2022, which noted “positive effects of mask mandates in the community setting and reductions in COVID-19 case growth, hospitalizations and deaths. However, there was limited evidence to suggest greater effectiveness of mask mandates when compared to mask recommendations for the outcome of COVID-19 case rate reduction.”
The scientists also looked to Google to find any polling done on the public acceptability of mask mandates.
They found a Forum Poll conducted on Nov. 8 that showed 53 per cent of respondents agreed that a mask mandate should be re-implemented in Ontario. They also found a Nanos Research poll conducted for CTV News from Oct. 30 to Nov. 2 that found 69 per cent of respondents would support the return of mask mandates to some extent.
The brief was never released publicly until The Canadian Press asked for it.
Public Health Ontario took a week to decide whether to release it, and the agency said it ultimately did in the interest of transparency. Public Health Ontario declined interview requests and only responded to questions through email.
“This document was not shared publicly as it was in response to a request from (Moore’s office) and not intended as a stand-alone document,” the email from PHO Media Relations said.
Moore did not answer a question about why the document was never made public.
The former scientific director of the old voluntary science table reviewed the brief after it was shared by The Canadian Press.
Dr. Fahad Razak called it an “even-handed assessment of the evidence.”
“It found what I believe to be true, which is that, in totality, the evidence suggests that masking does reduce spread in a school setting,” said Razak, an internist at St. Michael’s Hospital and a University of Toronto professor.
But Razak said the brief should have been made public when it was given to Moore in late November as debates around mask mandates swirled.
The former science table, which Public Health Ontario dissolved in September, published all of its work online at the same time it gave its reports and recommendations to the government, public health officials and the clinical community.
“As scientists and policy experts, we never believed that the decision was ours to make,” Razak said. “We believed that what was really important was providing timely information in a way that allowed best decisions to be made by the public and by decision makers,” he said.
Misinformation often occupies the space left in an information vacuum, Razak said.
“If you read the social media posts and the blogs and the concerns of people who distrust vaccines, for example, a lot of it stems from this idea that critical information is being kept behind closed doors,” he said.
“So that’s part of the thought process, which is driving misinformation and I think that’s one of the critical reasons why you want to establish transparency and timely reporting of data and analysis as a scientific body.”
The province’s new science table was formed under Public Health Ontario at the end of last year and Moore said it has only met a few times.
This report by The Canadian Press was first published Feb. 6, 2023.